Durable Medical Equipment (DME)
Simplify DME Billing and Maximize Cash Flow
Reduce denials, accelerate reimbursements, and improve cash flow with our specialized DME billing services. Let us handle the complexities, so you can focus on patient care.
Durable Medical Equipment (DME) billing services are important for healthcare providers and suppliers to manage the intricate processes of billing for medical devices and supplies. This specialized area of billing requires careful attention to detail to ensure claims are processed correctly, maximizing reimbursements.
Verifying insurance coverage, acquiring prior authorizations, and correctly using the Healthcare Common Procedure Coding System (HCPCS) and ICD-10 codes to prove medical necessity are among of the process’s most important elements. Reducing claim denials and delays requires accurate coding, accurate documentation of service dates, and patient records.
Submitting clean claims via Electronic Data Interchange (EDI) reduces errors and speeds up the payment process. Given the stringent regulations for Medicare and Medicaid, staying compliant with fee schedules and insurance protocols is critical to secure timely reimbursements. Outsourcing DME billing services can help alleviate administrative burdens, streamline operations, and enhance cash flow.
By prioritizing accurate coding, thorough documentation, and efficient claims management, DME billing services contribute to the financial stability of healthcare practices, allowing them to prioritize patient care. With over decades of expertise in the field, experienced DME billing companies play a crucial role in optimizing revenue cycles and minimizing financial losses for healthcare providers.
Take Control of Your Revenue Cycle
Managing Durable Medical Equipment (DME) billing can be challenging due to complex regulations and insurance requirements. Our experienced team simplifies the process, ensuring accurate coding, smooth claims submission, and faster reimbursements.
What Are DME Billing Services?
DME billing is the process of managing claims for medical equipment like wheelchairs, oxygen devices, CPAP machines, and other essential healthcare supplies. Our expert services ensure accurate billing, compliant coding, and efficient claims submission to reduce delays and denials.
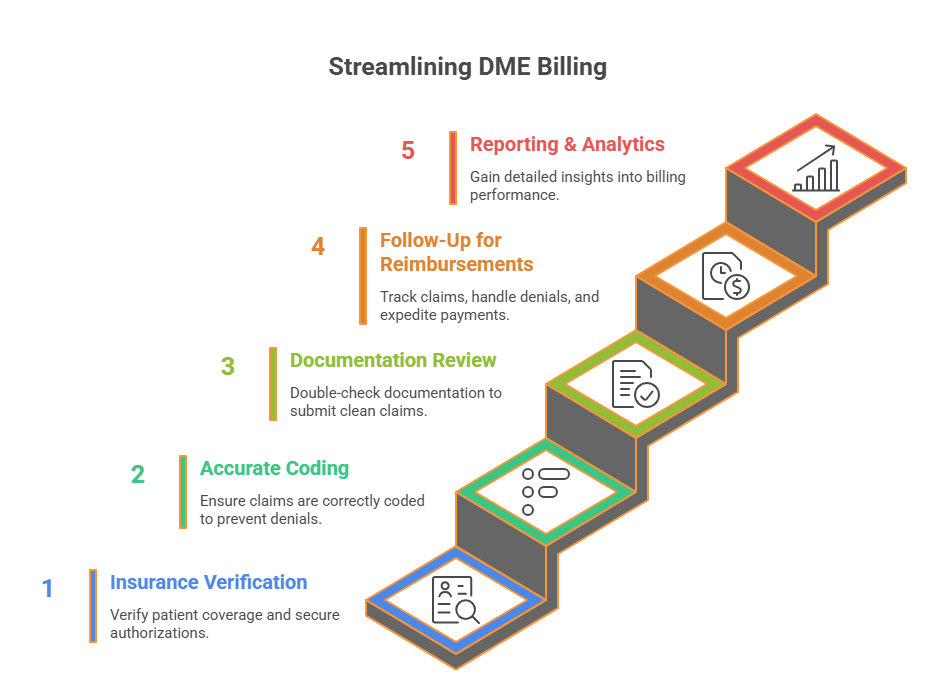
How Our DME Billing Process Works
Step 1: Insurance Verification & Prior Authorizations
Verify patient insurance coverage and secure necessary authorizations.
Step 2: Accurate Coding with HCPCS & ICD-10 Codes
Ensure all claims are correctly coded to prevent denials.
Step 3: Documentation Review & Claims Submission
Double-check documentation to submit clean claims quickly.
Step 4: Continuous Follow-Up for Reimbursements
Track claims, handle denials, and expedite payments.
Step 5: Reporting & Analytics for Financial Insights
Gain detailed insights into your practice’s billing performance.
Benefits of Partnering with Us
- Faster Reimbursements: Minimize delays with optimized claims processing.
- Increased Cash Flow: Improve revenue through accurate billing.
- Compliance with Regulations: Stay up-to-date with Medicare & Medicaid guidelines.
- Reduced Costs: Cut administrative expenses and enhance operational efficiency.
Our DME Billing Outsourcing Services
Running a medical supply business is tough, especially when dealing with the complicated world of billing for Durable Medical Equipment (DME). At AMedical Billing Services, Inc, we take that burden off your shoulders. By handling your DME billing process, we help you get paid faster, reduce billing errors, and improve your cash flow—all while letting you focus on what truly matters: patient care.
1. Checking Insurance Eligibility
Before supplying equipment, it’s crucial to confirm that a patient’s insurance will cover it. We handle the entire insurance eligibility check to make sure the patient qualifies for the equipment. This step helps avoid claims getting rejected later on.
2. Getting Prior Authorization
For some high-cost equipment, insurance companies need approval before you can provide it. We manage the prior authorization process for you, submitting the paperwork and following up to get it approved quickly.
3. Accurate Coding and Billing
Correct coding is key to getting paid. We have skilled professionals who know the latest DME billing codes (like HCPCS and ICD-10) inside and out. This ensures your claims are accurate and less likely to be rejected.
4. Submitting Claims
Submitting claims can be time-consuming, especially if done manually. We use advanced systems to submit your claims electronically, ensuring they’re processed quickly and correctly.
5. Handling Denied Claims
If your claim is denied or rejected, we don’t just stop there. Our team digs into the reason for the denial, fixes any issues, and takes appropriate actions.
6. Collecting Outstanding Balances
Once your claims are approved, you can rest assured that payment delays won’t be an issue. We proactively track and manage unpaid balances to ensure smooth and timely processing, so you don’t have to worry about a thing.
7. Fast and Accurate Payment Posting
When payments come in, they need to be posted accurately in your records. We make sure every payment is logged correctly and on time so your financial records are always up to date.
8. Reviewing and Auditing Claims
To mitigate potential issues with insurance companies, we conduct thorough reviews and audits of all claims before submission. This proactive approach helps identify discrepancies early and ensures compliance with insurance regulations.
Ready to Optimize Your DME Billing?
Schedule a free consultation to learn how we can reduce your claim denials and improve cash flow.
Why Partner with Us for DME Billing?
- Accurate Coding & Compliance: We stay up to date with HCPCS and ICD-10 codes to minimize errors and ensure accurate billing processes.
- Efficient Claims Processing: Clean claim submissions via Electronic Data Interchange (EDI).
- Reduced Administrative Burden: Focus on patient care while we optimize your billing process.
Why Choose Us for Your DME Billing?
Outsourcing your DME billing to AMedical Billing Services, means:
- Less Stress: We handle the complicated billing stuff so you can focus on your patients.
- Faster Payments: Reduce the time it takes to get paid and improve your cash flow.
- Fewer Errors: Our experienced team minimizes billing errors, helping to prevent delays in payment.
