Revenue Cycle Management
Revenue Cycle Management- An overview
Revenue Cycle Management (RCM) is the process of turning a patient visit into paid revenue for your practice. It covers every step—starting from the time an appointment is scheduled to when the final payment is collected.
The cycle includes:
- Checking insurance eligibility
- Recording charges and diagnoses
- Submitting claims to payers
- Following up on payments
- Handling denials and appeals
- Collecting balances from patients
- Reporting on cash flow and outstanding claims
RCM isn’t just billing. It’s a full system that keeps your practice financially healthy and your operations running smoothly.
The Importance of Revenue Cycle Management in Healthcare
Revenue Cycle Management is the backbone of healthcare finance. In a field where delayed Healthcare isn’t just about delivering care—it’s also about keeping your practice running. That’s where revenue cycle management (RCM) comes in. It’s the financial engine behind everything from paying your staff to investing in better equipment.
When RCM works, you get:
- Faster payments from insurance and patients
- Fewer denied or delayed claims
- Clear financial visibility
- More time for your team to focus on patient care
Poor RCM leads to
- High AR days (money stuck in limbo)
- Rejected or denied claims due to important errors
- Staff burnout from manual work and repeated follow-ups
- Lost revenue from missed deadlines or uncollected balances
Good RCM leads to
- Consistent cash flow
- Clean claims that are approved the first time
- Reduced workload for your billing team
- Better patient satisfaction due to fewer billing issues
It’s not just a back-end function—it’s the difference between a practice that struggles to stay afloat and one that runs efficiently, grows steadily, and delivers better care.
What Are the Steps in Revenue Cycle Management?
Understanding each stage of the revenue cycle is essential to optimizing it. Here’s a breakdown of the eight core phases involved in healthcare revenue cycle management:
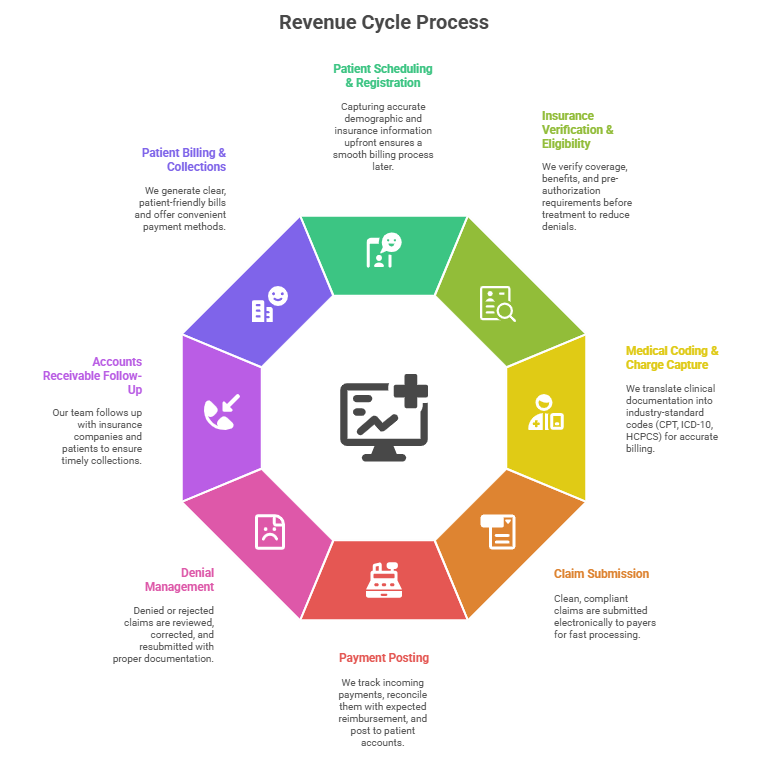
1. Patient Scheduling & Registration
Capturing accurate demographic and insurance information upfront ensures a smooth billing process later.
2. Insurance Verification & Eligibility
We verify coverage, benefits, and pre-authorization requirements before treatment to reduce denials.
3. Medical Coding & Charge Capture
We translate clinical documentation into industry-standard codes (CPT, ICD-10, HCPCS) for accurate billing.
4. Claim Submission
Clean, compliant claims are submitted electronically to payers for fast processing.
5. Payment Posting
We track incoming payments, reconcile them with expected reimbursement, and post to patient accounts.
6. Denial Management
Denied or rejected claims are reviewed, corrected, and resubmitted with proper documentation.
7. Accounts Receivable Follow-Up
Our team follows up with insurance companies and patients to ensure timely collections.
8. Patient Billing & Collections
We generate clear, patient-friendly bills and offer convenient payment methods.
At AMedical billing, every step is an opportunity to improve accuracy, speed, and profitability.
Challenges in Revenue Cycle Management
Revenue Cycle Management in healthcare is not without obstacles. Common challenges include:
- Claim Denials: Often due to incorrect coding, insufficient documentation, or missed deadlines.
- Regulatory Changes: Frequent updates in healthcare laws and payer policies.
- High Administrative Burden: Manual processes and lack of automation lead to inefficiency.
- Patient Payment Collection: Rising out-of-pocket expenses create collection difficulties.
- Data Silos: Disconnected systems lead to loss of crucial billing data.
These hurdles can be overcome with the right revenue cycle solutions that combine advanced technology, skilled professionals, and tailored strategies with AMedical billing.
Our End-to-End RCM Services
1. Patient Registration & Eligibility Verification
Before the visit, we verify insurance details, coverage limits, co-pays, deductibles, and pre-authorization requirements. This prevents delays later and ensures the patient is covered for the service.2. Medical Coding
Our certified coders translate procedures and diagnoses into the correct CPT, ICD-10, and HCPCS codes—minimizing claim errors and denials.3. Charge Entry
We input all billing information—accurately and quickly—into your system, ensuring the claim reflects the services provided.4. Claims Submission
We file clean claims to payers—on time and in compliance with insurer-specific rules. Fewer rejections, faster reimbursements.5. Payment Posting & Reconciliation
We match payments to claims, post them in your system, and reconcile against expected reimbursements. Any underpayments or discrepancies are flagged immediately.6. Denial Management & Appeals
We investigate denied claims, identify the cause, correct the issue, and resubmit or appeal with supporting documentation—maximizing recovery.7. Accounts Receivable (AR) Follow-Up
We track unpaid claims, follow up with payers, and push for resolution before claims age out. Regular AR reviews keep your cash flow steady.8. Patient Billing & Collections
We send out clear, easy-to-understand patient statements and follow up respectfully to collect outstanding balances—without harming the patient relationship.9. Reporting & Revenue Analytics
We provide custom reports on cash flow, AR trends, claim performance, and denial breakdowns—so you have full visibility and control. Whether you’re looking to fix specific gaps or offload your entire billing process, our RCM services are built to adapt to your workflow and scale with your practice.Who Can Benefit from Our RCM Solutions?
We serve a wide range of healthcare providers:
- Hospitals & Health Systems
- Ambulatory Surgery Centers (ASCs)
- Physician Practices
- Dental Clinics
- Urgent Care Centers
- Behavioral Health Providers
No matter your specialty, our tailored medical billing revenue cycle services can improve your bottom line.
How Can Revenue Cycle Management Be Improved?
Improving your healthcare revenue cycle involves a mix of technology, training, and process refinement:
- Automate Routine Tasks: Leverage AI and RPA for claim submission, eligibility checks, and payment reminders.
- Train Staff Continuously: Coding errors and front-desk mistakes are preventable with ongoing education.
- Track KPIs: Use performance indicators like Days in A/R, Clean Claim Rate, and Denial Rate to monitor progress.
- Partner with Experts: Outsourcing your RCM functions ensures consistency, compliance, and scalability.
Specialties We Serve
No two medical practices are the same. Each specialty comes with its own coding rules, documentation requirements, and payer challenges. We work with providers across a wide range of specialties—and tailor our RCM approach to fit yours.
Here are just some of the areas we support:
Primary Care
From preventive visits to chronic disease management, we ensure accurate coding and timely payments for all your routine and complex services.
Cardiology
We understand the detailed documentation and procedure-specific coding cardiology requires—including stress tests, EKGs, and interventional procedures.
Orthopedics
Whether you’re billing for fractures, joint replacements, or physical therapy, we handle surgical and non-surgical claims with precision.
Radiology
We manage billing for diagnostic imaging, CT, MRI, and interventional radiology—ensuring proper modifiers and payer-specific requirements are met.
Pediatrics
We take care of well-child visits, vaccinations, developmental screenings, and sick visits—handling the complexities of Medicaid and family insurance plans.
Mental Health & Psychiatry
We handle time-based codes, therapy session types, and telehealth billing, helping behavioral health providers get reimbursed fully and compliantly.
Surgery Centers
Our team is familiar with high-volume surgical billing, prior auth needs, and coding for bundled procedures in ASC settings.
Multi-Specialty Groups
We coordinate across departments and standardize billing workflows, so everything from internal medicine to specialty consults is billed cleanly under one roof.
How Our RCM Services Benefit You
Revenue Cycle Management isn’t just about fixing billing problems—it’s about building a system that works. Here’s what you gain when we manage your revenue cycle:
1. Faster Payments
We reduce delays by submitting clean claims and following up early. You get paid faster—by both payers and patients.
2. Fewer Denials
By verifying insurance, coding correctly, and tracking claims closely, we prevent denials before they happen and fix the ones that slip through.
3. Lower AR Days
With consistent follow-up and real-time tracking, we keep your Accounts Receivable under control. Less money stuck in the system means better cash flow.
4. Reduced Admin Work
Your staff won’t have to chase claims or juggle billing systems. We take that off your plate so your team can focus on patient care.
5. Clear Reporting
You’ll know exactly how your revenue is doing. No guesswork—just real numbers, updated regularly.
6. Scalable Support
Whether you’re adding new providers or expanding locations, our team scales with you. No disruption, no delays.
7. Stronger Compliance
We follow all payer rules and HIPAA standards, helping you stay audit-ready and avoiding penalties.
8. Happier Patients
Clear billing, fewer errors, and timely communication mean fewer complaints and better trust from your patients.
With the right RCM system in place, you’re not just collecting revenue—you’re creating stability for your practice to grow.
Why Choose Our RCM Company?
We combine over a decade of healthcare billing expertise with advanced analytics and unmatched customer service. Our Revenue Cycle Management team includes:
- Certified Professional Coders (CPC)
- Healthcare Compliance Officers
- Billing and A/R Specialists
- Denial Management Experts
What you get:
- Faster claims processing
- Fewer denials
- Better patient communication
Custom strategies tailored to your practice size and specialty
Our Technology & Tools
Efficient RCM isn’t just about good people—it’s about giving them the right tools. We use technology that speeds up claim handling, reduces human error, and gives your team full visibility into every step of the process.
Here’s what powers our work:
Claim Scrubbers
Before any claim goes out, we run it through automated scrubbers that catch coding issues, missing modifiers, and formatting errors. This improves your clean claim rate and reduces delays from rejections.
Eligibility & Benefits Verification Tools
We use integrated platforms to verify patient insurance coverage in real-time. This ensures services are authorized before the visit, avoiding unnecessary denials.
EHR and Billing System Integration
We work with most major EHRs and billing platforms—Athenahealth, eClinicalWorks, DrChrono, Kareo, AdvancedMD, and others. Our team adapts to your system so there’s no need for a major tech overhaul.
Denial Tracking Software
We track every denial by type, payer, and reason—so we know exactly where problems are happening and how to fix them. This helps reduce recurring issues over time.
Accounts Receivable Dashboards
You’ll get access to real-time AR dashboards showing claim status, collection timelines, and aging reports—broken down by payer, date of service, or provider.
Secure Document Management
All sensitive data is stored and shared through encrypted, HIPAA-compliant platforms. No email chains. No lost files. Everything is traceable and secure.
Custom Reporting Tools
Our reporting tools don’t just track what got paid—they show trends. We provide insights on denial causes, claim turnaround times, collection rates, and more.
Technology doesn’t replace expertise—but it makes it faster, more accurate, and easier to manage. And we make sure you always have access to the insights that matter.
FAQs About Revenue Cycle Management
1. What’s the difference between RCM and medical billing?
Medical billing is a part of RCM. RCM covers the entire process—from verifying insurance before a visit to collecting the final payment. It includes billing, coding, claim follow-up, denial handling, and reporting.2. Can I outsource only a part of my revenue cycle?
Yes. Some clients outsource just coding or denial management. Others hand over the entire cycle. We offer flexible plans so you can choose the level of support you need.3. Will I have to change my current EHR or billing system?
No. We work with your existing setup. Our team is trained on most major platforms and can integrate directly into your workflow.4. How do you make sure our data is safe?
We follow strict HIPAA protocols, use secure platforms, and have audit trails in place. Your patient data is encrypted, access-controlled, and fully compliant.5. What’s the benefit of outsourcing RCM instead of keeping it in-house?
Outsourcing reduces errors, speeds up collections, and frees up your staff. You also gain access to trained specialists and dedicated follow-up teams without hiring internally.6. How long does it take to see results?
Most clients see improvements in claim approval rates, AR days, and cash flow within the first 1–2 billing cycles. Denial recovery also picks up quickly once our system is in place.7. How do you handle denied claims?
We review the denial reason, correct the claim if needed, and resubmit or appeal with documentation. We also identify patterns to prevent the same issues from repeating.8. Can I see regular reports or updates?
Yes. You’ll get access to live dashboards and scheduled reports showing claims status, revenue trends, AR performance, and more.9. Do you handle patient billing and collections too?
Absolutely. We send timely, easy-to-understand statements to patients and follow up professionally to collect outstanding balances.10. Is there a long-term contract?
No. We offer flexible engagement options with no long-term lock-in. You continue with us as long as you’re happy with the results.Let’s Optimize Your Revenue Cycle Today
Struggling with denials, delayed payments, or rising overhead? Our comprehensive revenue cycle management services can help you regain control, boost profitability, and ensure compliance.
Contact us today for a consultation and customized revenue cycle audit.
